Diabetic Retinopathy
Definition
Diabetic retinopathy is a complication of diabetes mellitus (diabetes mellitus is a condition in which the blood sugar level is elevated because the body is unable to use and store sugar;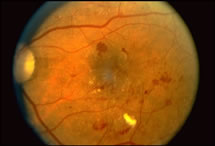 this high sugar content damages blood vessels in the body and can affect a variety of body organs such as the eyes, heart, and kidneys) and affects the eyes by causing deterioration of blood vessels in the retina. Abnormal retinal blood vessels may leak fluid or bleed or develop abnormal blood vessels that grow on the surface of the retina (neovascularization) and can bleed and scar. This can lead to loss of central and possibly peripheral vision.
this high sugar content damages blood vessels in the body and can affect a variety of body organs such as the eyes, heart, and kidneys) and affects the eyes by causing deterioration of blood vessels in the retina. Abnormal retinal blood vessels may leak fluid or bleed or develop abnormal blood vessels that grow on the surface of the retina (neovascularization) and can bleed and scar. This can lead to loss of central and possibly peripheral vision.
Causes and Associations
Diabetic retinopathy is caused by diabetes mellitus (diabetes mellitus is a condition in which the blood sugar level is elevated because the body is unable to use and store sugar; this high sugar content damages blood vessels in the body and can affect a variety of body organs such as the eyes, heart, and kidneys). The longer someone has diabetes mellitus, the more likely they will develop diabetic retinopathy. After 25 years, nearly all patients with diabetes mellitus will show some signs of diabetic retinopathy. A small number, however, will have a significant decrease in vision, and an even smaller number will go on to blindness.
The severity of diabetic retinopathy is also related to blood sugar control. The goal to reduce the rate of damage to the eyes, kidneys, and heart is a hemoglobin A1C level less than 7. Patients should discuss the hemoglobin A1C level with their medical doctors or diabetes mellitus specialist to try and achieve this goal. The hemoglobin A1C level reflects how well blood sugar control has been achieved over the past several months. The hemoglobin A1C numeric scale is different than the blood sugar numeric scale although laboratories are working to make them similar and easier to understand for patients.
Symptoms
Patients with diabetic retinopathy may notice no visual changes whatsoever. It is important and mandatory that patients with diabetes mellitus have their eyes examined at least annually. Progression of diabetic retinopathy and progression to vision loss may occur even when there are no symptoms.
The common symptoms of diabetic retinopathy include progressive blurring of vision; sudden, severe vision loss; floaters; or fluctuating vision.
Fluctuating vision may represent fluctuations in blood sugar level that can cause the lens of the eye to shrink and swell, thereby causing visual changes.
Examination
Complete and comprehensive ophthalmic examination is important in the assessment of diabetic retinopathy. Patients will receive vision testing, drops to dilate pupils, and a complete examination of the front and back of the eye. Pupillary dilation may create blurring, and therefore, it is often best if a driver accompanies the patient.
Testing
Patients with diabetic retinopathy may have several types of tests to assess their eyes:
- Fluorescein Angiography
Patients with diabetic retinopathy may undergo fluorescein angiography to assess blood flow in the retina or to assess for leakage or bleeding that may lead to vision loss. Fluorescein angiography is performed by injecting sodium fluorescein dye into a peripheral vein with a small needle; this dye then goes through the body and eyes, as well as the retina, to assess blood flow and determine where areas of leakage are located. It may be performed to assess whether there is evidence of diabetic retinopathy. It is regarded as a safe test, but patients should expect some yellowish skin discoloration and orange urine. Most patients have no difficulty with this testing, although a low percentage of patients will experience some nausea. Any angiogram test, however, can be associated with allergic or even more severe reactions, and therefore, this test is reserved for patients in whom diabetic retinopathy is noted or suspected. - Fundus Photography
Patients may also undergo fundus photography to document the stage and findings of diabetic retinopathy. This procedure is of little risk to the patient. - OCT Imaging:
OCT imaging is a non-invasive optical coherence tomogram examination of the macula; an OCT uses a low energy laser to scan the macula and determine whether there is leakage or swelling within the macula, potentially signifying diabetic retinopathy. It can help assess the status of the macula and retina in patients with diabetic retinopathy. It can monitor swelling in the macula that can lead to vision loss and can also identify areas of attachment of the vitreous gel to the retina. OCT imaging may be performed to monitor treatment for diabetic macular leakage or to evaluate the attachment of the vitreous gel to the retina over time.
What the Doctor Sees
There are two major types of diabetic retinopathy: non-proliferative retinopathy and proliferative retinopathy:
- Non-proliferative Diabetic Retinopathy
Non-proliferative diabetic retinopathy is characterized by damage to small retinal blood vessels that typically cause bleeding or leakage. These blood vessels may develop balloon-like swelling called microaneurysms. Microaneurysms and other areas of abnormal retinal blood vessels may leak fluid, causing the retina to swell or bleed. This may lead to vision loss. Leakage in the macula, known as macular edema, is the most common mechanism of vision loss in patients with non-proliferative diabetic retinopathy. Non-proliferative diabetic retinopathy is the most common form of diabetic retinopathy, accounting for approximately 80% of all cases. - Proliferative Diabetic Retinopathy
Most patients never progress beyond non-proliferative diabetic retinopathy, however some patients may progress to proliferative diabetic retinopathy. Proliferative diabetic retinopathy is characterized by significant loss of blood flow to the retina by capillary blood vessel occlusions. Capillaries comprise the smallest blood vessel networks in the body and are found throughout the body and in the retina. This creates an oxygen deficiency in the retina which then stimulates the growth of abnormal new blood vessels on the surface of the retina and the optic nerve, as well as other structures in the eye. These abnormal blood vessels are fragile and can bleed and scar, thereby causing significant hemorrhage and sudden loss of vision. Vitreous hemorrhage may cause sudden and acute painless loss of vision characterized by cobwebs and then diffusely smoky vision. Patients with this type of vision loss should be evaluated promptly by an ophthalmologist.Proliferative diabetic retinopathy can also lead to scarring of the abnormal blood vessels growing on the surface of the retina. This can lead to contraction of scarring on the surface of the retina and retinal detachment. Retinal detachment can lead to loss of reading vision if it involves the macula, or that part of the retina which is responsible for central vision.
Prognosis
Patients who maintain healthy, active lifestyles and who optimize their blood sugar control have the best chance of preserving good vision. It is very important that patients with diabetes mellitus undergo at least an annual eye exam, whether or not they have vision problems. Remember, diabetic retinopathy may progress and not cause any symptoms. It is also very important for patients to understand that their blood sugar control should be as good as possible with the goal of a hemoglobin A1C level less than 7. A hemoglobin A1C level higher than 7 should prompt a discussion with medical doctors on how to improve blood sugar control.
Prevention and Treatment
- Laser Photocoagulation
Laser Photocoagulation is a proven treatment for diabetic retinopathy. A laser delivers a split-second burst of intense light energy to treat leaky blood vessels or areas of low blood flow in eyes with diabetic retinopathy. Laser photocoagulation has significantly reduced the chance of blindness in patients with diabetic retinopathy.Laser photocoagulation is performed in the office setting with the patient seated in front of the laser unit. The eye is anesthetized with drops, and a contact lens in placed on the eye to focus the laser-aiming beam. Patients will experience bright flashes of lights and occasionally a pinching sensation, although many patients will have no sensation of the laser at all. Some patients may experience discomfort during laser photocoagulation, but generally it is a well tolerated office procedure.
- Laser Light
Laser Light is used to treat leaky blood vessels, as well as to treat areas of low blood flow in the retina to reduce the stimulus for abnormal blood vessel growth, bleeding, and scarring. - Steroid Injections or Avastin
Many retina specialists are now using injection therapies into the eye to try and treat complications of diabetic retinopathy such as leakage and abnormal blood vessel growth. Steroid injections or Avastin may be injected into the eye after topical anesthetic and sterilization. These injections are associated with a small risk of hemorrhage or infection, and therefore, patients are typically treated with topical antibiotic drops. Avastin is designed to shrink blood vessels and therefore shrinks certain cancer tumors after injection of the drug in a peripheral vein.Steroid injections also may be associated with elevating the pressure of the eye or causing progression of cataract. Patients should discuss risks and benefits of all treatments, including injection therapies, with their eye specialist.
- Vitrectomy
Patients with diabetic retinopathy may require cutting surgery in an operating room setting. A vitrectomy is performed when there is bleeding or scarring that causes loss of vision in patients with advanced diabetic retinopathy. In this surgical procedure, small instruments are inserted into the eye under microscopic visualization, and both the vitreous hemorrhage and scarring are removed and replaced with clear fluids. Laser photocoagulation may be performed at the time of surgery, and in some cases, a long-acting gas bubble or silicone oil may be placed to hold the retina in position and to reduce bleeding. The prognosis for patients who require vitrectomy surgery depends upon the status of the underlying diabetic retina.Diabetic Retinopathy
Author: Allen C. Ho, M.D.